Development of a sophisticated artificial pancreas holds potential to transform the lives of patients with Type 1 diabetes.
Type 1 diabetes is a lifelong condition caused when the pancreas stops producing the insulin needed to control blood sugar levels. Patients must carry out frequent finger-prick tests and inject insulin to keep their blood sugar within safe limits.
Left untreated, Type 1 diabetes is fatal; even suboptimal control increases the risk of heart disease, stroke, kidney failure, nerve damage and blindness. Patients under the age of five are a particularly vulnerable group. Too young to recognise the shaking and dizziness that warn of a drop in their blood sugar, they are at high risk of developing overnight hypoglycaemia.
By maintaining tight control of blood sugar, this has the potential to revolutionise the treatment of patients with Type 1 diabetes and significantly improve their quality of life.
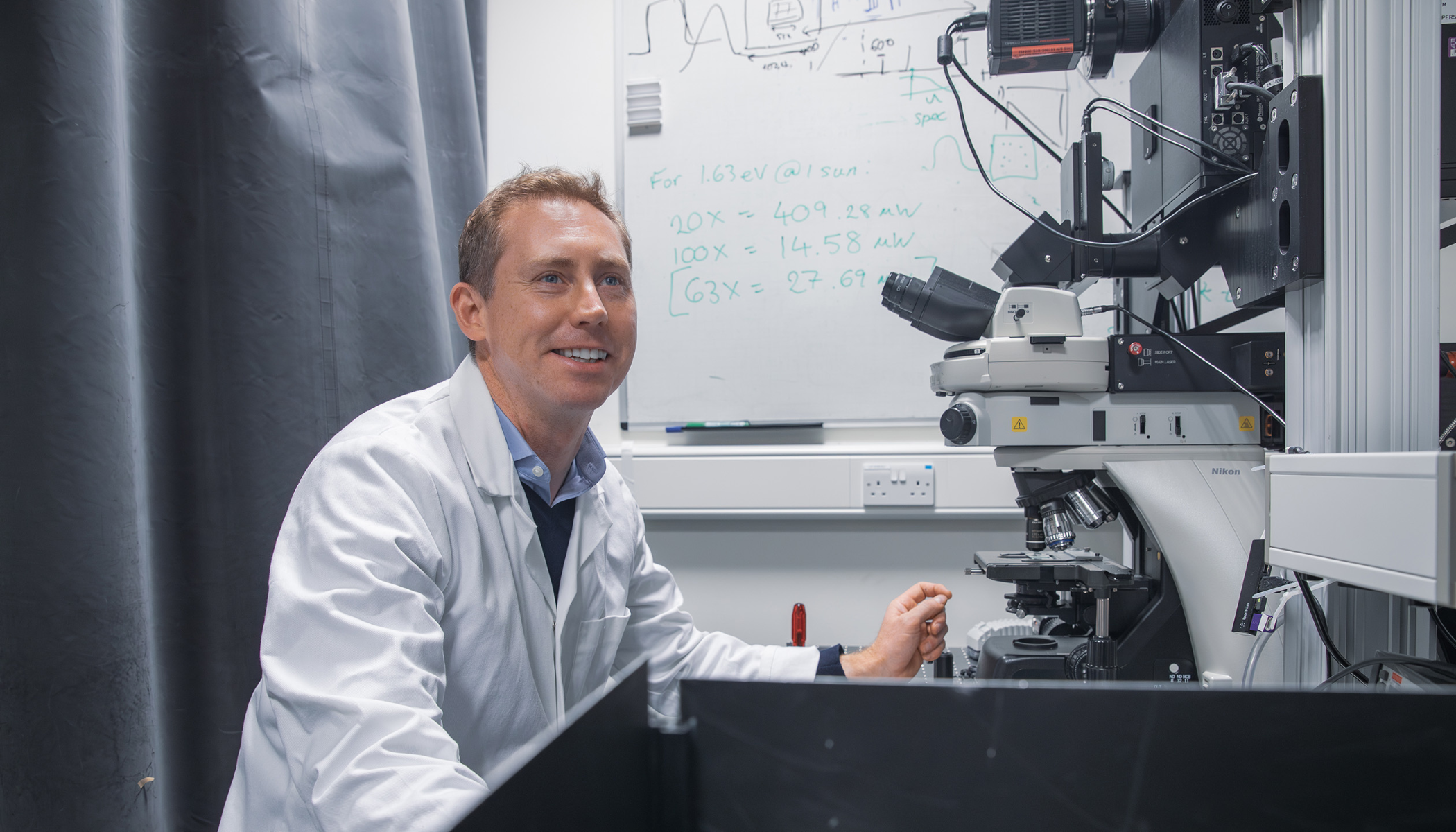
Dr Roman Hovorka
Now, a clinical trial with this age group is testing an ‘artificial pancreas’, developed by the group of Dr Roman Hovorka, Director of Research at the University’s Metabolic Research Laboratories. “Using an off-the-shelf insulin pump and continuous glucose sensor, we’ve developed a computer algorithm to control their function in a closed-loop fashion, delivering the correct amount of insulin according to blood sugar levels,” he said. “By maintaining tight control of blood sugar, this has the potential to revolutionise the treatment of patients with Type 1 diabetes and significantly improve their quality of life.”
The glucose-responsive insulin delivery system has been trialled in adolescents, adults and pregnant women with Type 1 diabetes at the Cambridge Clinical Research Facility (CRF), and follow-on studies are ongoing with these groups at home.
Hovorka has now turned his focus towards using the system to help the very youngest patients. This year, 78,000 children worldwide were diagnosed with Type 1 diabetes, and the incidence in under-fives is rising annually by 3% in many countries.
“The risk of these children developing overnight hypoglycaemia, when blood glucose levels drop dangerously low and can lead to a coma, is a major concern for parents,” said Hovorka. “The tiring routine of getting up several times every night to check their child’s blood sugar is disruptive for the whole family.”
In the new trial, running until July 2013, children stay overnight at the CRF with their parents. “Insulin is a hormone that is powerful enough to kill people, so we need to be very careful,” said Hovorka, whose research is funded by the Juvenile Diabetes Research Foundation, US National Institutes of Health, Diabetes Research Network, National Institute for Health Research (NIHR), Diabetes UK and European Commission. “Our trials at the CRF are an essential step, enabling us to document safety and reliability with different groups before we let them test it at home. Our controlled conditions, and proximity to the hospital, provide reassurance that, if there is a problem, we can help.”
The CRF is a joint venture between the University’s School of Clinical Medicine, the NIHR and the Wellcome Trust. It provides facilities for investigators from across the Cambridge Biomedical Campus to carry out clinical trials in patients and healthy volunteers, but is now greatly oversubscribed. Fundraising is currently under way to enable an extension to be built next year, to accelerate the development of effective new treatments and interventions to benefit patients across a wide range of conditions, including obesity and diabetes, immune and inflammatory disorders, and cancer.
For Hovorka, various other trials of the artificial pancreas system are also in progress, including in the control of blood sugar in patients in the Neurosciences Critical Care Unit at Cambridge University Hospitals NHS Foundation Trust, and his prototype devices are being commercialised by Cambridge Enterprise, the University’s commercialisation arm. “We hope to make the overnight closed-loop system widely available in the next three to five years,” he said.
This article appears in the latest edition of Research Horizons, the University’s research magazine.