The culmination of three decades of research in Cambridge has resulted in the exciting prospect of a new transformational treatment for multiple sclerosis.
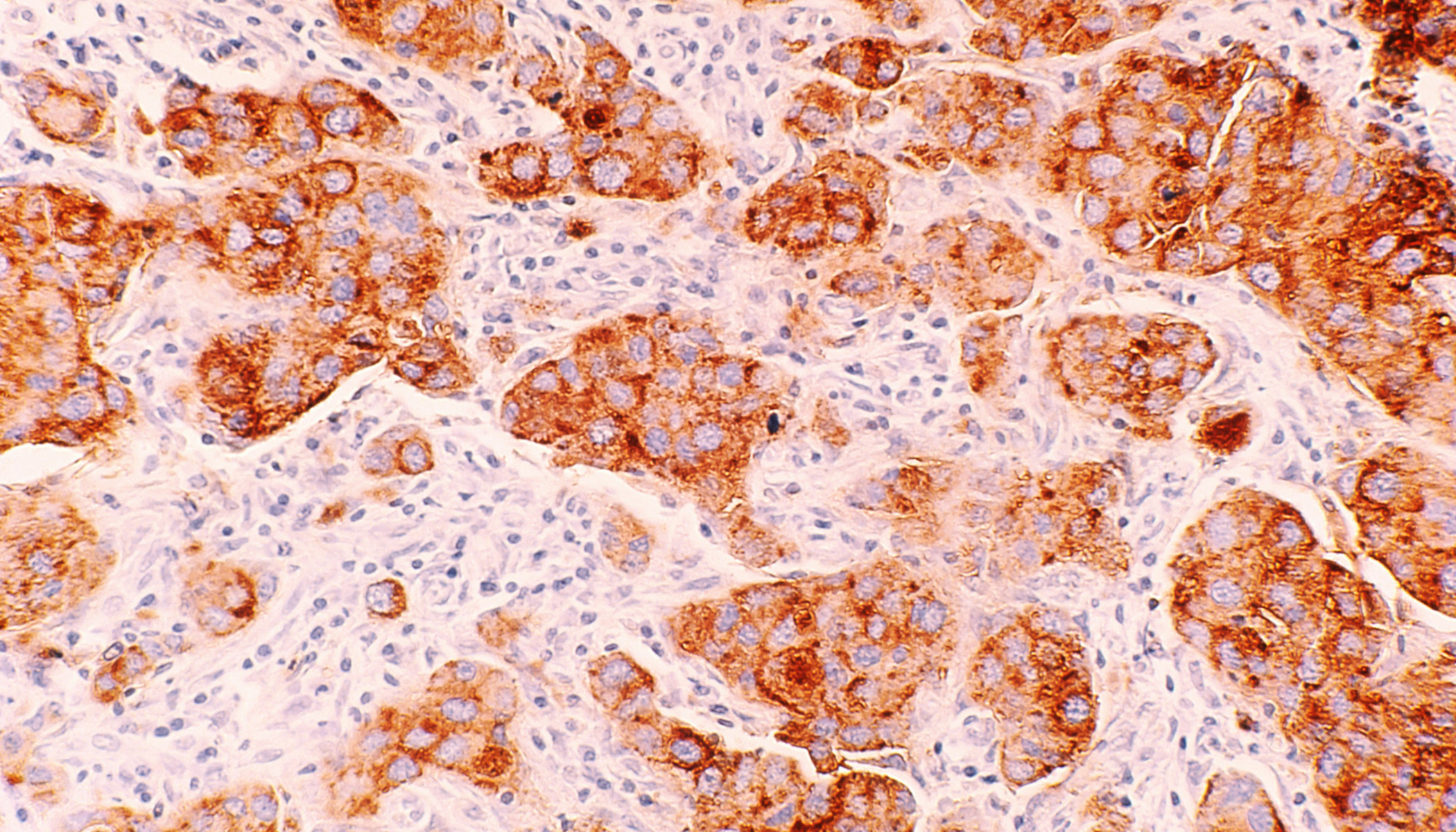
In 1975 Cambridge scientists Cesar Milstein and George Kohler at the Laboratory for Molecular Biology (LMB) invented the technology to make large quantities of a monoclonal antibody of any specificity, for which they would later receive the Nobel Prize for Physiology or Medicine. Building on this research, Herman Waldmann, Geoff Hale and Mike Clark, University of Cambridge, with Greg Winter and Lutz Riechmann, LMB, produced the first humanised monoclonal antibody for use as a medicine, Campath-1H (now known as alemtuzumab).
Taken together, the phase II and III clinical trial data illustrate the promise that alemtuzumab holds as a transformative treatment for a broad range of people with relapsing multiple sclerosis.
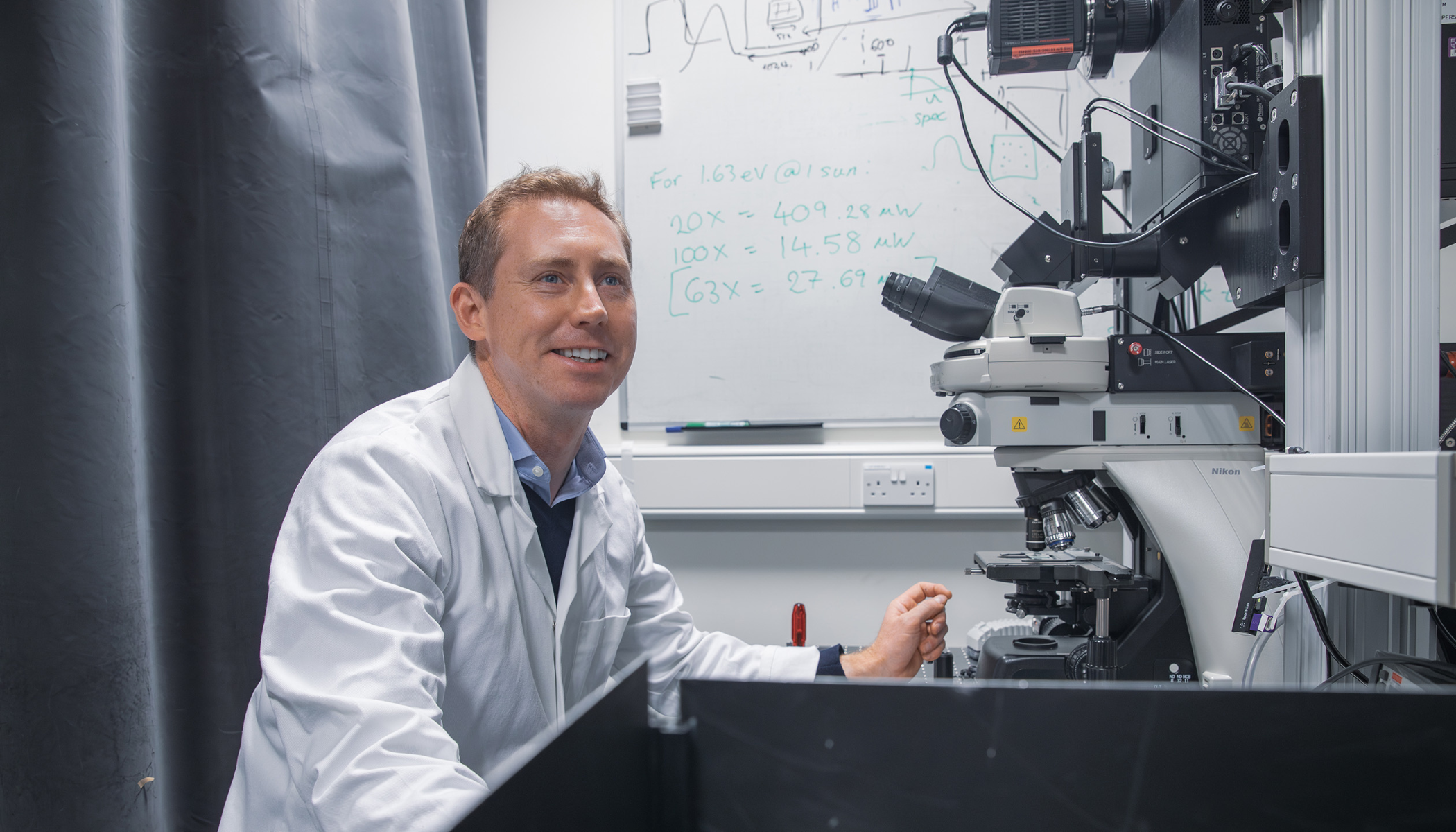
Professor Alastair Compston
Campath-1H was licensed for the treatment of chronic lymphocytic leukaemia, but in the 1980s Cambridge clinical scientists also began to explore its use in diseases where the immune system is overactive.
In 1991, Professor Alastair Compston (current Head of the Department of Clinical Neurosciences) began to explore the use of alemtuzumab as a treatment for the autoimmune disease multiple sclerosis. He and Dr Alasdair Coles (currently University Lecturer in the same department), led the subsequent phases of development of alemtuzumab in multiple sclerosis, in a fruitful partnership with the company Genzyme, now a Sanofi company. In 2008, they announced the results of a phase 2 trial and, in October 2011, they reported the results of the first of two phase 3 trials (CARE-MS1).
Today, Monday 14 November, the successful top line results from the second of the two Phase III trials (CARE – MS2) were announced. The trial was overseen by Professor Compston as the Chair of the Steering Committee.
“CARE-MS2 represents the culmination of many years clinical and laboratory research aimed at demonstrating the potential for alemtuzumab as a highly effective treatment for multiple sclerosis and understanding mechanisms involved in the complex natural history of the disease,” said Professor Alastair Compston, Chair of the Steering Committee overseeing the conduct of the study. “Taken together, the phase II and III clinical trial data illustrate the promise that alemtuzumab holds as a transformative treatment for a broad range of people with relapsing multiple sclerosis.”
Dr Alasdair Coles said: “Three important results emerge from these trials. First, they show that just eight days of alemtuzumab significantly reduces the risk of having another relapse of multiple sclerosis or becoming disabled over the next 3 to 5 years, compared to the standard active drug, interferon-beta. Secondly, many patients on alemtuzumab experience an improvement in disability, which is not seen after standard treatment. Finally, although alemtuzumab causes potentially serious side-effects, these can be identified and treated provided a monitoring schedule is carefully followed.”
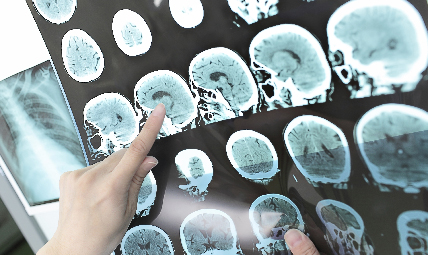
Multiple sclerosis is an autoimmune disease, in which the body’s immune system mistakes friend as foe. Immune cells mistakenly attack nerve fibres and their protective insulation, the myelin sheath, in the central nervous system. The resulting damage prevents the nerves from ‘firing’ properly and ultimately leads to their destruction, resulting in physical and intellectual disabilities.
“Alemtuzumab works by inflicting a short sharp shock to the immune system, by depleting a key cell type called lymphocytes, which then ‘reboot’, leading to a modified immune repertoire that no longer regards myelin and nerves as an invading bug. In so doing, roughly one third of patients after alemtuzumab develop another autoimmune disease, mainly against the thyroid gland and rarely against platelets in the blood,” explains Dr Coles.
Dr Coles’ research team is investigating how to detect people who are susceptible to this particular side-effect, with generous funding from the Grand Charity of the Freemasons, UK and the Evelyn Trust. Additionally, the Moulton Charitable Trust and the Medical Research Council have agreed to fund a trial of alemtuzumab in combination with a novel drug to reduce the risk of autoimmune disease. (Several years ago, the Moulton Charitable Trust also funded Dr Coles’ group to test a strategy to reduce the chance that the immune system will “reject” alemtuzumab after multiple doses.)
It is hoped the drug will be approved by the UK and US regulatory bodies in the next two years, concluding the 36 year epic journey from fundamental research to a new, effective treatment for MS.
Multiple sclerosis affects almost 100,000 people in the United Kingdom, 400,000 in the United States and several million worldwide. Symptoms of the disease can include loss of physical skills, sensation, vision, bladder control, and intellectual abilities.